never beat within a human breast"
- Lord Byron
1957-2010
With and Without
Doug died unexpectedly at the age of 52 while running.
Doug was very active. He ran 3.5 to 5 miles a day. On June 8, 2010, after had gone about 1.75 miles and showed no signs of distress, he split off from his running buddies to go back to the office. His heart stopped. It was apparently not a heart attack, stroke or aneurysm. Medics reached him within maybe 4 to 5 minutes but were unable to revive him.
The ER doctor thought the cause was probably a malignant heart arrhythmia triggering sudden cardiac arrest (basically stopping his heart). The cause of Doug's untimely death was listed on the death certificate "hypertensive cardiovascular disease." The medical examiner found:
- Concentric atherosclerotic coronary artery wall thickening. (Atherosclerosis is a type of arteriosclerosis, where fatty material collects along the arterial walls and hardens.)
- Cardiomegaly (heart weight of 490 grams)
- Left ventricular hypertrophy (left ventricle 1.8 cm) (This actually showed up on an EKG shortly before his collapse.)
- (The second and third conditions could be associated with an athletic lifestyle.)
- Read more.
No other problems were found. According to the Mayo Clinic website:
"Sudden cardiac arrest usually results from an electrical disturbance in your heart that disrupts its pumping action and causes blood to stop flowing to the rest of your body. Sudden cardiac arrest is different from a heart attack, which occurs when blood flow to a portion of the heart is blocked, depriving the heart muscle of necessary oxygen. Like a heart attack, however, sudden cardiac arrest almost always occurs in the context of other underlying heart problems, particularly coronary artery disease.
Sudden cardiac arrest symptoms are sudden and drastic: ■ Sudden collapse ■ No pulse ■ No breathing ■ Loss of consciousness. Sometimes, other signs and symptoms precede sudden cardiac arrest. These may include fatigue, fainting, blackouts, dizziness, chest pain, shortness of breath, palpitations or vomiting. But sudden cardiac arrest often occurs with no warning."
Doug's recent EKG's did show sinus bradycardia (a heart rate under 60), but this is often dismissed in athletes. It is a sign of being very fit. However, it can also be caused by:
- diseases that damage the heart's electrical system
- electrolyte imbalance (too much potassium in the blood.) Doug's 4/2010 blood test showed normal levels of potassium, but Benicar can affect potassium levels.
- high blood pressure medicines, in particular beta blockers, antiarrhythmics and digoxin. Doug was on a different kind - an ARB - see more below.
WHAT CAUSED HIS HEART TO STOP?
The question is what caused sudden cardiac arrest. The Mayo Clinic website indicates that:
"The most common cause of cardiac arrest is an arrhythmia called ventricular fibrillation — when rapid, erratic electrical impulses cause your ventricles to quiver uselessly instead of pumping blood. Without an effective heartbeat, your blood pressure plummets, cutting off blood supply to your vital organs. Most of the time, cardiac-arrest-inducing arrhythmias don't occur on their own. In a person with a normal, healthy heart, a sustained arrhythmia is unlikely to develop without some outside trigger, such as an electrical shock, the use of illegal drugs, or trauma to the chest at just the wrong time of the heart's cycle (commotio cordis)."
In Doug's case, there was no trauma. He did not use ANY illegal drugs. He never smoked. He was at an ideal weight. He regularly monitored his blood pressure. He ate lots of vegetables, fruit and protein. He exercised regularly. He slept about 8 to 9 hours a night.
He was regularly taking prescription medications for hypertension and elevated cholesterol. He also took an aspirin a day, and sometimes a multi-vitamin.
However, his heart was not normal, as the autopsy noted.
 BENICAR & BENICAR HCT
BENICAR & BENICAR HCT
If you have experienced an adverse reaction while taking Benicar, you can report it to the FDA on Medwatch.
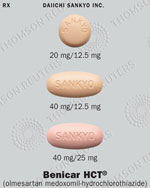
Doug had borderline hypertension, and was on Benicar HCT 40-12.5 since September 2009.
Benicar HCT® (olmesartan medoxomil-hydrochlorothiazide) is a combination of an angiotensin II receptor antagonist (AT1 subtype), olmesartan medoxomil, and a thiazide diuretic, hydrochlorothiazide (HCTZ). Benicar HCT went on the market in 2003, after being tested for just 8 weeks in clinical trials of about 1200 patients.
Doug was also taking Crestor to lower his cholesterol. He also had slightly impaired fasting glucose (blood sugar) levels. His physician said that, had he lived longer, he might have eventually developed diabetes.
While on Benicar, Doug experienced shortness of breath and fatigue. My husband was quite athletic. He ran 4 to 5 days a week, had completed 6 marathons, and regularly hiked and climbed rock, ice and mountains. He felt the symptoms he was experiencing were associated either with the Benicar HCT, Crestor or the combination. (His father was also having the same symptoms, and demanded that his doctor take him off Benicar after Doug died. His father immediately felt better. And his blood pressure didn't change (he was also on another blood pressure medication). Same thing for the father of my friend J.)
Doug's MD decided he should continue taking it after a treadmill test done a few months after Doug started taking Benicar.
Doug had a fainting incident three months before he died while running. The doctor did an ECG, and concluded that Doug was probably dehydrated (even though he didn't experience symptoms like nausea before fainting.) In hindsight, it was more than that. the doctor had him continue to take Benicar.
After Doug died, I learned that one of his parents has a gene that impairs the body's ability to metabolize drugs. For these kinds of people, drugs can stay in the system longer, and be more toxic. This may have been a factor for Doug.
If you are currently on Benicar or Benicar HCT (especially if you are diabetic), I URGE you to talk to your prescribing physician about alternatives and monitoring. See the FDA Drug Safety Communication: Ongoing safety review of Benicar and cardiovascular events, issued three days after Doug's death, and make sure your doctor reviews it.
This announcement deals with two large, long term (39 months) clinical trials were held where people with Type 2 diabetes (which Doug did not have) received either Benicar or a placebo. The unexpected result was that diabetics taking Benicar were ~3-5 times more likely to die from a cardiac event than were those taking a placebo.
FDA documents indicate the following about Benicar HCT:
"Interference with adequate oral electrolyte intake will also contribute to hypokalemia. Hypokalemia may cause cardiac arrhythmia and may also sensitize or exaggerate the response of the heart to the toxic effects of digitalis (e.g., increased ventricular irritability)."
"Cardiovascular side effects of olmesartan have been reported in 0.5% to 1% of patients, including tachycardia, chest pain, and peripheral edema. Symptomatic hypotension may occur in volume- or salt-depleted patients. .... Cardiac arrhythmias, including ventricular ectopy and complete AV heart block, are associated with hypokalemia and hyponatremia due to hydrochlorothiazide (HCTZ). Hypotension has been reported in association with HCTZ-induced pulmonary edema. Orthostatic hypotension may occur and may rarely be associated with syncope [fainting], particularly in the elderly."
On 4/11/2011, the FDA issued an update:
After reviewing the results of the ROADMAP and ORIENT trials,1-2 FDA has determined that the benefits of Benicar continue to outweigh its potential risks when used for the treatment of patients with high blood pressure according to the drug label2. Benicar is not recommended as a treatment to delay or prevent protein in the urine (microalbuminuria) in diabetic patients. Patients should consult their health care professional if they have any questions or concerns about taking Benicar. Daiichi Sankyo, the makers of Benicar, have agreed to work with the FDA to perform additional studies, as well as conduct additional analyses of completed clinical studies, to obtain more complete information about the cardiovascular risks or benefits of Benicar in various clinical settings. FDA will update the public when new information is available.
The Mayo Clinic did a study where there appeared to be a connection between Benicar and celiac disease symptoms. They concluded that Olmesartan may be associated with a severe form of spruelike enteropathy, which can cause electrolyte imbalances. Read study. Electrolyte imbalances can associated with cardiac arrhythmia.
ABOUT HYPERTENSION
According to NPR, hypertension, or high blood pressure, is the second leading cause of death in the U.S., and is a major risk factor for heart disease and strokes. As the pressure gets higher, it begins to damage the walls of the blood vessels.
An estimated 1 in 3 adults has high blood pressure. NIH guidelines specify that a blood pressure of 120/80 is normal. Blood pressure consistently over 140/90 is considered hypertension. Even on Benicar HCT, Doug's blood pressure measured 142/89 (on average over 65 measurements.) When he was younger, Doug had hypertension and was on Beta Blockers for several years. Then he was able to reduce his high blood pressure by losing weight and exercising regularly. It started to creep back up in 2005 or 2006. He did not smoke. He took a baby aspirin every day. He was doing everything right.
STRESS TESTS
See Demystifying the Cardiac Stress Test, Hartford Courant, 02/22/2010. "Exercise stress tests are only about 60 percent effective, meaning they miss 40 percent of the problems."
In November 2009, Doug underwent a treadmill test administered by a cardiologist.
- Exercise stress test: (Also called treadmill test, exercise test and exercise cardiac stress test): Doctors monitor your EKG while you're at rest and when you're working hard, such as walking on a treadmill or riding a stationary bike. Good for: Picking up blockages greater than 70 percent; showing how much you can safely do after a heart attack or surgery.
Doug did not have any of the other tests listed below, other than EKGs in the MD's office. I was not aware that he was not given an echocardiogram by the cardiologist until after his death. From the article:
- Electrocardiogram (EKG or ECG): Records the heart's electrical activity and shows abnormal heart rhythms. Can show a heart attack in progress. Good for: Showing whether a heart attack has occurred, Predicting whether one is developing, Monitoring a change in heart rhythm. A lot of people confuse an EKG with an ECHOcardiogram.
- Echocardiogram: An ultrasound for the heart. Patients exercise on a treadmill or bike but instead of using the EKG, doctors place a handheld device on the chest to create video pictures of the heart's chambers, valves, wall motion and blood flow patterns. Good for: Assessing heart health, including abnormal rhythms (arrhythmia) in the heart. For women, it's slightly more accurate than an exercise stress test.
- Cardiac computerized tomography (CT) or magnetic resonance imaging (MRI). Although more commonly used to check for heart failure, more doctors are using these tests to diagnose heart problems. In a cardiac CT scan, you lie on a table inside a doughnut-shaped machine called a gantry. An X-ray tube inside the machine rotates around your body and collects images of your heart and chest. In a cardiac MRI, you lie on a table inside a long tube-like machine that produces a magnetic field. The magnetic field aligns atomic particles in some of your cells. When radio waves are broadcast toward these aligned particles, they produce signals that vary according to the type of tissue they are. Images of your heart are created from these signals, which your doctor will look at to determine the cause of your enlarged heart.
- Blood tests. Your doctor may order blood tests to check the levels of certain substances in your blood that may signal that you have an enlarged heart. Blood tests can also help your doctor rule out other conditions that may cause your symptoms.
- Cardiac catheterization and biopsy. In this procedure, a thin tube (catheter) is inserted in your groin and threaded through your blood vessels to your heart, where a small sample (biopsy) of your heart can be extracted for analysis in the laboratory. Pressure within the chambers of your heart can be measured to see how forcefully blood pumps through your heart. Pictures of the arteries of the heart can be taken during the procedure (coronary angiogram) to ensure that you do not have any blockage.
- Chest X-ray. X-ray images help your doctor see the condition of your lungs and heart. If your heart is enlarged it might first be detected by a chest X-ray, but other tests will usually be needed to find out the specific cause. Your doctor can also use an X-ray to diagnose conditions other than enlarged heart that may explain your signs and symptoms.
There are other tests too, such as nuclear medicine, wearing a Holter monitor to check for abnormalities etc.
Some of all of these tests might have revealed what was wrong with Doug.
SEARCHING FOR ANSWERS AND LESSONS LEARNED
In the midst of angst about why this had to happen to Doug, I'm trying to focus sometimes on lessons learned that might help others.
Lessons learned for me:
- Be your own medical advocate.
- Don't allow your spouse to dismiss concerns. (Of course, Doug often dismissed MY concerns about many things - including his health. Recently, I had yelled at him for dismissing my concerns about him dismissing my concerns :-) The doctor DID tell him to listen to his wife ....
- Try this: A person I met recently, whose husband didn't want to deal with some medical issues, said she told him "If you love me, you will take care of yourself."
- Never stop searching for answers if you suspect something is really wrong.
- Be aware of all the side effects of drugs so you can be on the lookout.
- Be aware of signals that something is wrong (such as excessive tiredness, which I attributed to stress at work and Doug's non-stop physical activity.)
- Demand more tests if you learn they might be helpful.
- Get a second opinion.
LINKS to more information. Hindsight is 20-20.
- FDA Drug Safety Communication: Ongoing safety review of Benicar and cardiovascular events
- Report adverse reaction to Benicar to the FDA
- Cardiovascular Events Trigger FDA Review of ARB, MedPage Today, 06/11/2010 by Peggy Peck
- ROADMAP trial
- ORIENT trial
- Benicar and Benicar HCT and arrhythmia
- FDA info on Benicar and side effects
- Ventricular Arrhythmias, HeartPoint
- Arrhythmias and Sudden Cardiac Death, American Heart Association
- Demystifying the Cardiac Stress Test, Hartford Courant, 02/22/2010.
- Sinus bradycardia
- Benicar HCT contains a diuretic. One of the side effects of diuretics is arrhythmia. See WebMD.com. Other possible side effects include faintness (Doug had a fainting incident in March. The doctor concluded it was possibly due to dehydration and a vasovagal syncope (blood pooling when they stopped suddenly while running to give someone directions.) In hindsight, it might have been an arrhythmia. Another documented side effect is excessive sweating. Doug's sweating during running increased after going on Benicar HCT. Also muscle cramps, which Doug experienced more of in bed. It can also cause a potassium imbalance. The excessive sweating combined frequent urination caused by the diuretic and a potassium imbalance can cause problems.
- Heart Disease & Abnormal Heart Rhythm, WebMD.com Shortness of breath and fatigue can be indicators of arrhythmia. This was a common complaint for Doug while on Benicar HCT. Arrhythmia can be diagnosed by several tests. The only ones Doug was given were short-term EKG's and a stress test. Beta blockers can be used to treat this condition (as well as hypertension), but Doug was prescribed a different kind of hypertension medication called an ARB. Beta blockers have a whole different set of side effects.
- Stimulants can make arrhythmias worse. Doug did not smoke or use any stimulants like cough or cold medications. He did drink small quantities of caffeine coffee (a few cups in the morning.) Doug was taking an aspirin a day (81 mg.) He cut back on caffeine after the fainting incident, and was eating breakfast daily. He usually had a banana (a good source of potassium) almost every day. Sometimes he remembered to take a Flintstone's multi-vitamin.
- Mode of action - From HealthSquare.com: "Benicar controls high blood pressure. It works by blocking the effect of a hormone called angiotensin II. Unopposed, this substance prompts the blood vessels to contract, an action that tends to raise blood pressure. Benicar relaxes and expands the blood vessels, allowing pressure to drop. Benicar may be prescribed alone or with other blood pressure medications, such as diuretics that help the body get rid of excess water. Benicar HCT provides just such a combination. It contains Benicar plus hydrochlorothiazide, a common diuretic that increases the output of urine. This removes excess fluid from the body and helps lower blood pressure."
- Malignant Arrhythmias: Life-threatening arrhythmia is uncommon (5.7%) with Apical Ballooning Syndrome (ABS) despite marked, structural abnormalities. When arrhythmias do occur, the outcome is poor.
- Medline Search, Benicar
- Drug interactions- HERG & arrhythmia
- Mayo Clinic, Sudden Cardiac Arrest and Arrhythmias
- Benicar and Benicar HCT are marketed by Daiichi Sankyo, Inc., which has a U.S. headquarters in Parsippany, N.J.
- Sudden death - what it is like for those left behind
- The end - what happened to Doug
- Malignant arrhythmias and sudden cardiac arrest
- Dealing with a death that was preventable (07/28/2012)
©2010. Designed by Chimalis LLC.
Please request permission before re-publishing content from this website, except for content on the quotes/poems page. This website is not intended as a substitute for the medical advice of physicians. The reader should regularly consult a physician in matters relating to his/her health and particularly with respect to any symptoms that may require diagnosis or medical attention. The author shall have neither liability nor responsibility to any person or entity with respect to any loss, damage or disruption caused, or alleged to have been caused, directly or indirectly, by any information contained on this website.